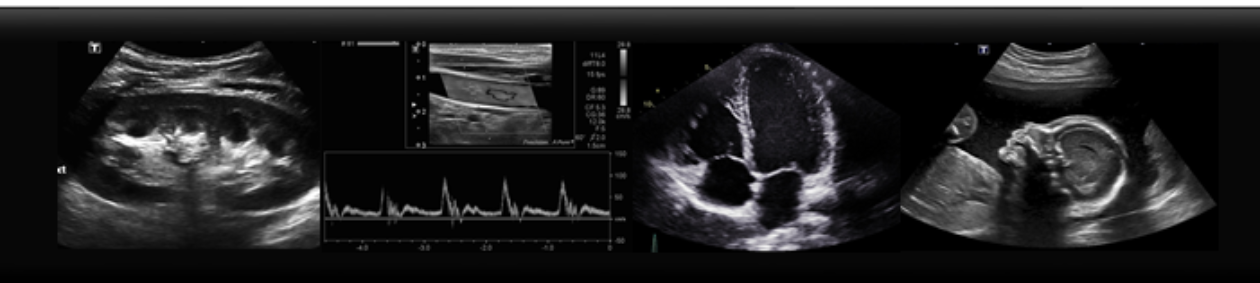
On ultrasound, vessels look black, or anechoic, due to the fact that they are fluid filled. You can also use colour Doppler to see the flow of blood within these vessels.
Holding your probe in transverse on the patient’s leg, find the common femoral artery and vein at the proximal thigh. By applying firm pressure with the probe to the patient, the vein should easily collapse. Follow the vein from the thigh to behind the knee, to the popliteal vein.

However, if the vein does not compress, this should raise suspicion for a DVT. Often, you will be able to see clot within the vein, as the vessel is no longer anechoic, but filled with hypoechoic clot. Also, if you turn on colour Doppler there will be no colour flow within the vessel.


Images:
http://www.nuemblog.com/dvt
https://radiopaedia.org/cases/lower-limb-deep-venous-thrombosis-dvt